Neuralgia literally means nerve (neur-) pain (algia). Nerve pain is usually sharp and shocking, and may be combined with pins and needles, numbness, weakness. Sometimes it is associated with unusual sensations like running water or insects crawling on the skin (paraesthesia). Your GP may prescribe painkillers to help manage symptoms, because nerve pain is often unresponsive to paracetamol or ibuprofen.
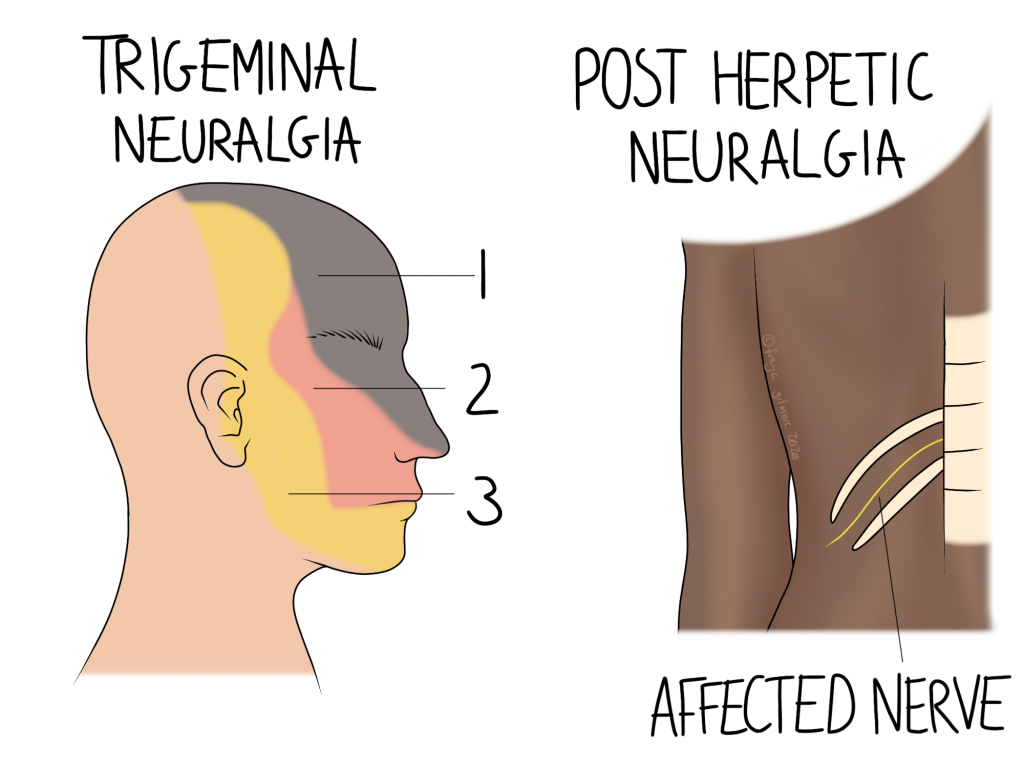
Two relatively common forms of neuralgia are trigeminal neuralgia and postherpetic neuralgia.
Trigeminal Neuralgia (TN)
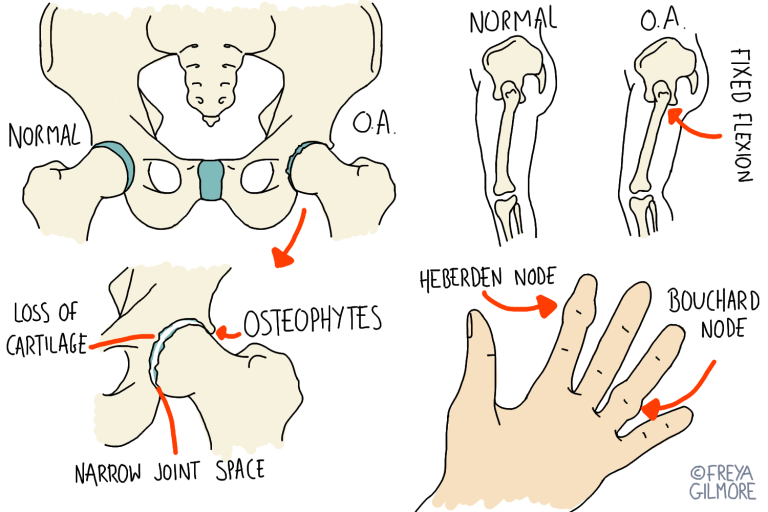
The trigeminal nerve is a nerve that supplies the face. The “tri” in its name refers to the three branches it splits into on either side of the head. Illustrated above, they are:
- orbital (top of head, eyes, most of the nose)
- maxillary (mid face)
- mandibular (jaw to temple)
TN usually affects one branch, but sometimes multiple are involved. In any case, symptoms come in the form of an attack, with sharp shooting pain appearing in the area supplied by the nerve. An attack can last a few seconds or a few minutes, and low level symptoms may follow its resolution. Something as innocuous as a breeze on the face can set one off, making it potentially very debilitating. It is not unusual for someone with TN to also struggle with tension in the neck and shoulders which may lead to headaches.
Post-Herpetic Neuralgia
Shingles, caused by the herpes zoster virus, can cause neuralgia after the initial infection. Active shingles typically cause pain along the course of a nerve, along with a chicken pox type rash. Often the nerves between ribs are affected, as illustrated above, but any nerve can be affected. You’re less likely to develop post-herpetic neuralgia if you have the shingles vaccine, or if you take antiviral medication from your GP during an episode of shingles.
As the rash and other symptoms begin to fade, you may be left with lasting nerve pain in the same area. Another symptom is itchiness, or sensitivity to things like clothes or bedsheets on skin.
Desensitising a Nerve
With both conditions mentioned above, there is often no physical cause for the pain. TN can be caused by pressure where the nerve exits the skull, but this is not always the case. If we are dealing with pain without stimulus, the key is to desensitise the nerve.
Nerve pain like this is exacerbated by the brain’s need to keep us safe. At one point, the brain perceived a threat, but it hasn’t yet turned off the alert. This is not to say that your symptoms are your fault or even made up- this is a subconscious process. Your osteopath’s job is to convince the brain to turn off the alarms and bring the pain levels down. We can use techniques to move associated joints gently, and apply gentle stimuli to the skin. By gradually increasing the input here, we can raise the brain’s threshold for what should be felt as pain.
It’s a slow and steady process, and may work well with medication prescribed by your GP. Every case is different, and your treatment plan will be tailored to your case specifically, but we are more than happy to work alongside other healthcare professionals.
Click here to make an appointment in the Bristol area for your neuraglia